The Genetics of Sleep Apnea: A Comprehensive Guide

Sleep Apnea is a multifactorial sleep disorder that impacts millions globally. Though lifestyle and environmental components determine its onset, studies indicate there is a strong genetic connection.
Types of Sleep Apnea:
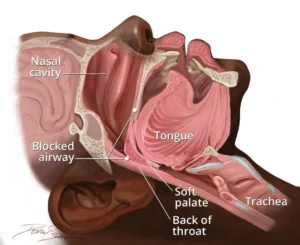
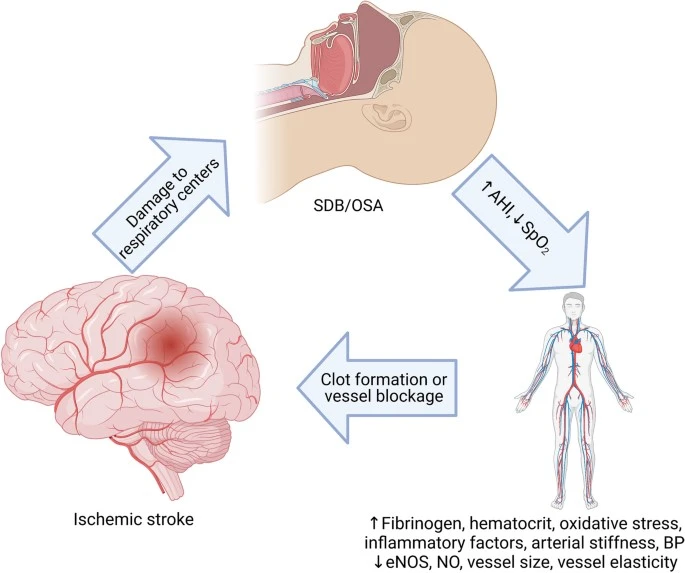
- Obstructive sleep apnea: Upper airways becomes blocked many times you sleep, this can block the airways. This is also known to be as Obstructive sleep apnea (OSA), airways get narrow by various factors like obesity, large tonsils, or changes in your hormone.
- Central sleep apnea: In this type of sleep apnea brain doesn’t send the signal, needed to breath. Health gets affected.
Mixed sleep apnea: It is the combination of Obstructive sleep apnea (OSA), and Central Sleep Apnea (CSA).
Cause of Sleep Apnea:
Sleep Apnea may be induced by following factors:
- Airway obstruction: When muscles in the throat relax, the airway becomes narrowed or Collapses.
- Brain signaling problems: Difficulty with brain’s ability to transmit signals to breathing-controlling muscles.
- Obesity: Excess weight may lead to sleep apnea.
- Airway anatomy: Narrow airway, broad tonsils, and broad tongue may cause sleep apnea.
- Age: Sleep apnea is most likely to occur in old people.
- Family History: If in a family any of individual is with sleep apnea condition then the there are high chances of developing the sleep apnea condition. Research indicates that sleep apnea found to be linked with certain genetic variants, especially those related to be linked with certain genetic variants, especially those related to breathing control and airway structure.
Smoking and Nasal Congestion: Smoking and nasal congestion are both linked to an increased risk and severity of sleep apnea. Smoking contributes to upper airway inflammation and swelling, potentially narrowing the airways and making them more prone to collapse during sleep. Nasal congestion, whether due to anatomical issues or allergies, can also worsen sleep apnea by forcing individuals to breathe through their mouths, which may not be as effective at maintaining an open airway.
Symptoms
- Breathing that starts and stops
- Frequent loud snoring
- Gasping for air
- Daytime sleepiness and tiredness, which can lead to problems with learning, focusing, and reacting
- Dry mouth
- Fatigue
- Headache
- Insomnia Sexual dysfunction or decreased libido
- Waking up often during the night to urinate
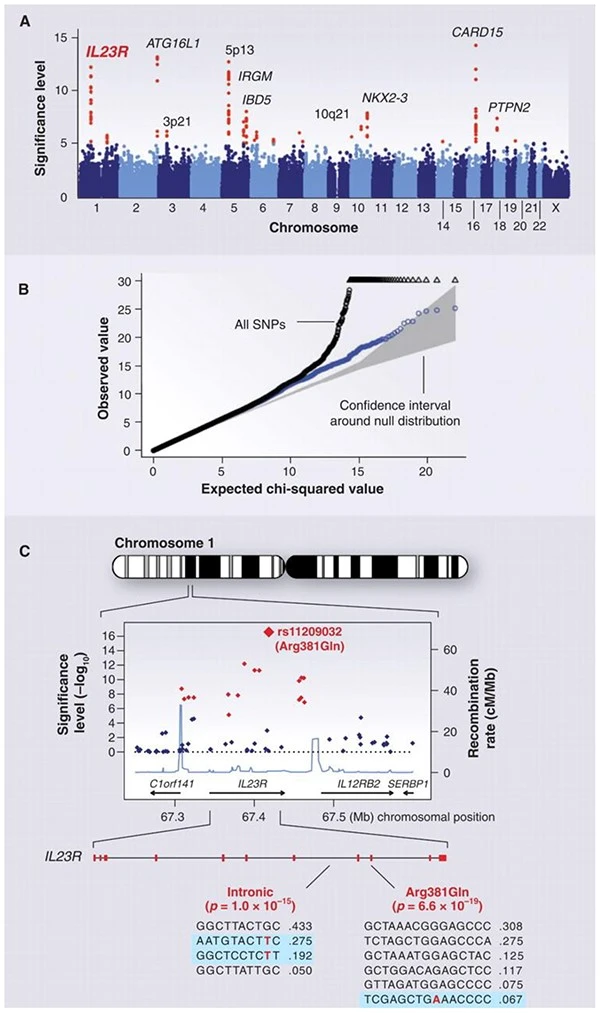
Analytic approaches to detect genes for complex diseases such as Obstructive Sleep Apnea (OSA)
To detect genes associated with obstructive sleep apnea, researchers use various analytical approaches:
- Genome-wide association studies (GWAS)
- Linkage analysis
- Candidate gene approach
- Exome sequencing
- Bioinformatics analysis
Best sellers
-
Modavinil 200mg
$69.00 – $395.00Price range: $69.00 through $395.00Shop Now This product has multiple variants. The options may be chosen on the product page -
Modafil Md 200 mg
$69.00 – $345.00Price range: $69.00 through $345.00Shop Now This product has multiple variants. The options may be chosen on the product page -
Modvigil 200mg
$65.00 – $395.00Price range: $65.00 through $395.00Shop Now This product has multiple variants. The options may be chosen on the product page -
Vilafinil 200 mg
$69.00 – $395.00Price range: $69.00 through $395.00Shop Now This product has multiple variants. The options may be chosen on the product page -
Modalert 200 mg
$69.00 – $449.00Price range: $69.00 through $449.00Shop Now This product has multiple variants. The options may be chosen on the product page -
Modafresh 200 mg
$65.00 – $329.00Price range: $65.00 through $329.00Shop Now This product has multiple variants. The options may be chosen on the product page
This approaches help researchers:
- Identify genetic variant associated with OSA.
- Understand the biological mechanisms underlying OSA.
- Develop genetic risk scores for OSA prediction.
Inform personalized treatment strategies.
Biomarker’s used:
Biomarkers are the biological indicators that are used to diagnose, monitor, and predict the disease:
- C-reactive protein (CRP)
- Interleukin-6 (IL-6)
- Tumor necrosis factor-alpha (TNF-alpha)
- Leptin and ghrelin
- Oxidative stress markers
- Genetic markers
Risk Factors:
It can affect anyone. Specific risk factors are:
- Narrow airway
- Family history
- Alcohol & tranquilizers consumption
- Smoking
- Prior medical condition
- Nasal Congestion
Diagnosis:
Sleep apnea is typically diagnosed through sleep studies,
- In a sleep lab (Polysomnography): This is the best way of diagnosing sleep apnea. During a PSG, sensors are attached to the body to monitor brain activity, heart rate, breathing patterns, and blood oxygen levels while you sleep.
- At home (Home sleep apnea testing): This involves using a portable device at home to monitor breathing patterns, oxygen levels, and heart rate during sleep. It is a convenient alternative to in-lab testing, especially for those with suspected uncomplicated obstructive sleep apnea.
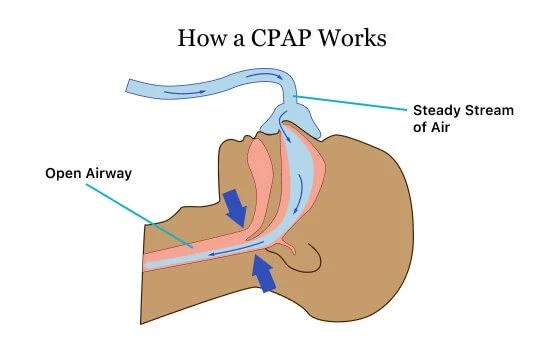
CPAP Treatment:
Continuous Positive Airway Pressure (CPAP) is a treatment that uses a machine to deliver pressurized air through a mask to keep the airways open during sleep, primarily used for sleep apnea. It helps prevent airway collapse, thereby improving breathing and sleep quality.
How does CPAP work?
Continuous flow of air is generated by motor of CPAP Machine, then delivered the users through mask. Depending upon preferences mask can be used like, nasal mask (covering the nose), a full-face mask (covering both nose and mouth), or nasal pillows (small inserts for the nostrils).
Healthcare professional sets machine at specific pressure. CPAP does not breathe for the user, it simply maintains the airway open to facilitate normal breathing.
Pros of using CPAP treatment
- Reduce risk of health problems.
- Improves sleep Quality.
- Reduce day time sleepiness.
- Improves concentration and memory.
- Lowers blood pressure
Cons of CPAP treatment
- Noise
- Claustrophobia
- Mask discomfort
Other treatments
- Mandibular advancement devices (MADs)
- Tongue-retaining devices
- Uvulopalatopharyngoplasty (UPPP)
- Genioglossal advancement
- Hyoid Suspension
- Positional theory
- Nasal strips
- Expiratory positive airway pressure (EPAP) devices
- Upper airway stimulation
- Hypoglossal nerve stimulation
Conclusion:
Sleep apnea is a significant health concern that requires proper management and attention, also need to study genetics of sleep, do not ignore symptoms, consult a physician immediately after getting any of the above symptoms. It is recommended to have a healthy diet to get rid of obesity, regular exercise, and avoid alcohol. Also keep your nasal passage open while you sleep. Biomarkers like C-reactive protein (CRP), Interleukin-6 (IL-6), Tumor necrosis factor-alpha (TNF-alpha), Leptin and ghrelin, oxidative stress markers etc can be use to diagnose sleep apnea, monitor treatment, and also predict the outcomes.
References
FAQs
- What do you mean by sleep apnea?
Sleep Apnea is a multifactorial sleep disorder that impacts millions globally. Though lifestyle and environmental components determine its onset, studies indicate there is a strong genetic connection.
- Sleep apnea can be treated completely?
Not all type of sleep apnea are treated as Obstructive sleep apnea is chronic and permanent conditions but still it can be treated by several surgeries and proper medications.
- Is sleep apnea genetic?
Yes, sleep apnea is genetic, If in a family any of individual is with sleep apnea condition then the there are high chances of developing the sleep apnea condition.
- Which can be the best way of diagnosing sleep apnea?
Polysomnography is the best way of diagnosing sleep apnea. During a polysomnography, sensors are attached to the body to monitor brain activity, heart rate, breathing patterns, and blood oxygen levels while you sleep.
- What do you mean by CPAP treatment?
Continuous Positive Airway Pressure (CPAP) is a treatment that uses a machine to deliver pressurized air through a mask to keep the airways open during sleep, primarily used for sleep apnea. It helps prevent airway collapse, thereby improving breathing and sleep quality.